
31 Jan GLP-1 Drugs Explained: What You Need to Know
Last update: February 1, 2026 | Author: Siri Napan, MD
You’ve probably heard about Ozempic, Wegovy, or Mounjaro—medications that are changing the landscape of diabetes and weight management. These drugs belong to a revolutionary class of medications called GLP-1 receptor agonists (and their cousins, the GLP-1/GIP dual agonists). This guide will help you understand how they work, who they’re for, and what to expect.
Understanding GLP-1
GLP-1 stands for glucagon-like peptide-1, a hormone your body naturally produces in your intestines after you eat. Think of it as one of your body’s natural appetite and blood sugar regulators. When you eat a meal, GLP-1 tells your brain you’re full, signals your pancreas to release insulin (which lowers blood sugar), and slows down how quickly food moves through your stomach.
The problem? Natural GLP-1 breaks down in your body within minutes. Scientists created medications that mimic GLP-1 but last much longer—hours or even days instead of minutes. This extended action is what makes them so effective for managing diabetes and weight.
How Do GLP-1 Agonists Work?
These medications work in several ways at once:
-
- Reduce hunger: They work on your brain’s appetite centers, helping you feel fuller with less food and reducing cravings
- Slow digestion: They slow down how quickly your stomach empties, keeping you satisfied longer after meals
- Improve blood sugar control: They help your pancreas release the right amount of insulin when you eat, and prevent your liver from making too much sugar
- Protect your heart: Research shows many of these medications reduce the risk of heart attacks and strokes
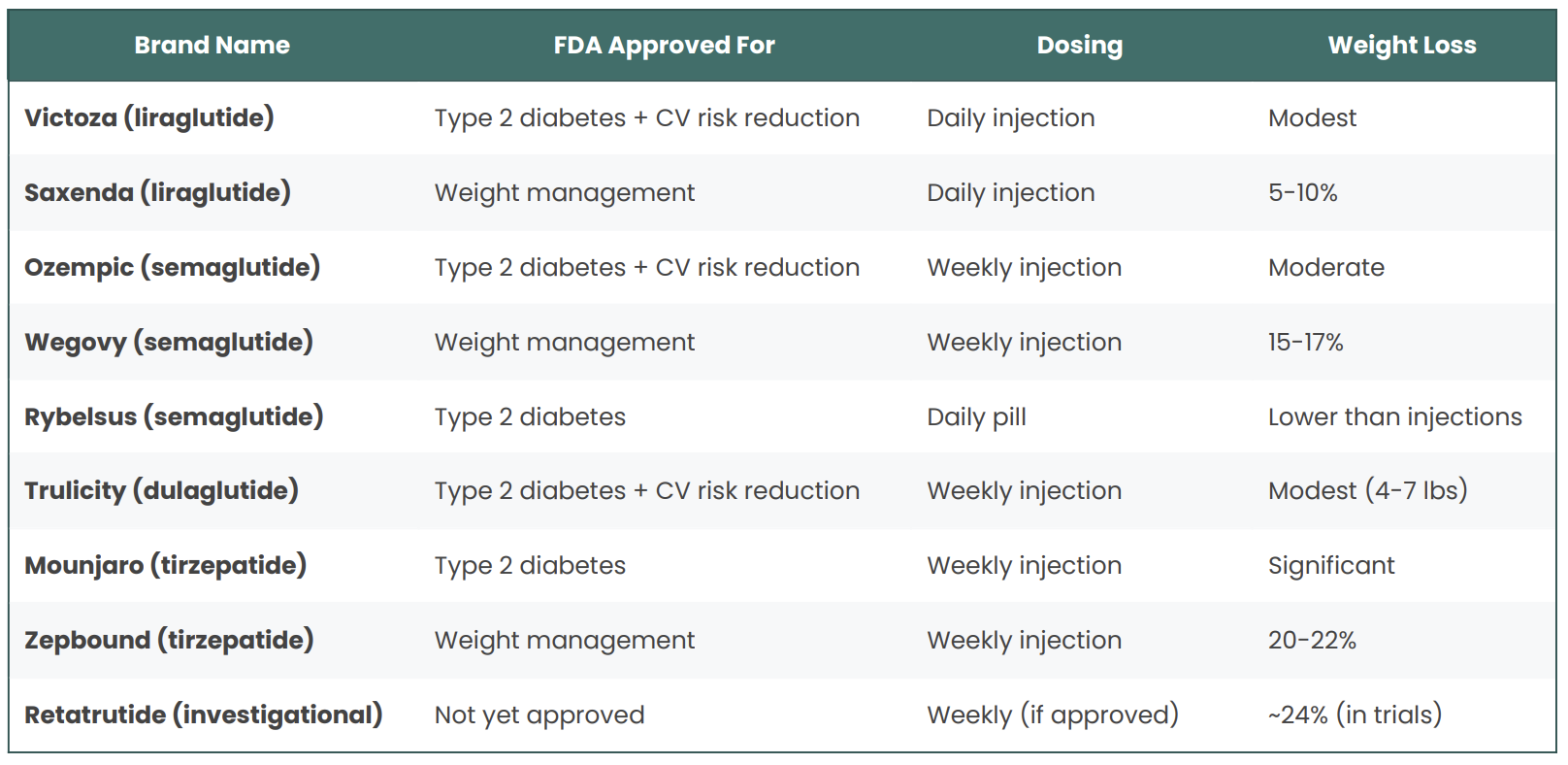
The Main Players: Currently Prescribed Medications
While several GLP-1 medications have been developed over the years, these are the ones most commonly prescribed today:
Liraglutide (Victoza®, Saxenda®)
How it works:
Mimics the GLP-1 hormone to reduce appetite, slow digestion, increase insulin release, and lower blood sugar.
What it’s approved for:
- Victoza: Type 2 diabetes + heart risk reduction
- Saxenda: Weight management
How it’s taken:
Daily injection
What to expect:
- A1C reduction: ~1–1.5%
- Weight loss: ~5–10% of body weight
- Proven heart protection in people with diabetes
Good to know:
This is one of the oldest GLP-1 drugs, so doctors know it well. Daily injections are less convenient than weekly options.
Common side effects:
Nausea, vomiting, diarrhea, constipation, headache
(Usually improve over time)
Rare but serious:
Pancreatitis, gallbladder issues, thyroid tumors (seen in animals)
Semaglutide (Ozempic®, Wegovy®, Rybelsus®)
How it works:
Strong GLP-1 activation that suppresses appetite, slows stomach emptying, improves insulin response, and lowers blood sugar.
What it’s approved for:
- Ozempic: Type 2 diabetes + heart risk reduction
- Wegovy: Weight management
- Rybelsus: Type 2 diabetes (oral pill)
How it’s taken:
- Ozempic / Wegovy: Weekly injection
- Rybelsus: Daily pill (empty stomach, wait 30 minutes before eating)
What to expect:
- A1C reduction: ~1.5–2%
- Weight loss (Wegovy): ~15–17% of body weight
- Strong heart protection
Good to know:
Weekly dosing is convenient. The pill avoids needles but is less effective and harder to take correctly.
Common side effects:
Nausea, vomiting, diarrhea, constipation, stomach pain
Rare but serious:
Pancreatitis, gallbladder disease, thyroid tumors, delayed stomach emptying
Dulaglutide (Trulicity®)
How it works:
GLP-1 activation that improves insulin release, reduces appetite, and slows digestion.
What it’s approved for:
Type 2 diabetes + heart risk reduction
How it’s taken:
Weekly injection (very easy pen, no visible needle)
What to expect:
- A1C reduction: ~0.8–1.6%
- Weight loss: modest (4–7 lbs)
- Proven heart benefit
Good to know:
Often chosen for simplicity and safety in people with kidney disease.
Common side effects:
Nausea, diarrhea, reduced appetite
Rare but serious:
Pancreatitis, thyroid tumors, kidney issues
Tirzepatide (Mounjaro®, Zepbound®)
Mechanism (how it works):
Activates two hormones:
- GLP-1 → appetite control, insulin release
- GIP → enhances insulin response and fat loss
This dual action makes it more powerful than GLP-1 alone.
What it’s approved for:
- Mounjaro: Type 2 diabetes
- Zepbound: Weight management
How it’s taken:
Weekly injection
What to expect:
- A1C reduction: ~2–2.5%
- Weight loss: ~20–22% of body weight
- Some people reach near-normal blood sugar
Good to know:
This is currently the strongest approved option. Long-term heart outcome data is still ongoing.
Common side effects:
Nausea, vomiting, diarrhea, constipation, very low appetite
Rare but serious:
Pancreatitis, gallbladder disease, thyroid tumors, delayed stomach emptying (~10% stop due to GI side effects)
Retatrutide (Investigational – Not Yet Approved)
How it works:
Activates three hormones:
- GLP-1 → appetite suppression
- GIP → insulin sensitivity
- Glucagon → increases energy use and metabolism
This triple action increases fat loss and calorie burning.
Approval status:
Not FDA-approved (Phase 3 trials)
How it would be taken:
Weekly injection
What studies show:
- Weight loss: ~24% of body weight
- Results approach weight-loss surgery outcomes
Good to know:
Not available yet. Likely 2026 if approved. Long-term safety still being studied.
Side effects seen in trials:
Similar GI effects as other GLP-1 drugs (nausea, vomiting, diarrhea)
Who Should Consider These Medications?
For Type 2 Diabetes
These medications are approved for adults with type 2 diabetes who need help managing their blood sugar. They work particularly well if:
- Your A1C is still too high despite lifestyle changes and other medications
- You want to avoid or reduce insulin
- You have heart disease or are at high risk for it
- Weight loss would benefit your overall health
For Weight Management
For weight loss, these medications are approved for adults with:
- A BMI of 30 or higher (obesity), OR
- A BMI of 27 or higher (overweight) plus at least one weight-related health condition like high blood pressure, high cholesterol, or sleep apnea
Some formulations are also approved for adolescents aged 12 and up who meet certain criteria.
Who Should NOT Take These Medications
These medications aren’t for everyone. You shouldn’t take them if you:
- Are pregnant, trying to get pregnant, or breastfeeding
- Have a personal or family history of medullary thyroid cancer
- Have Multiple Endocrine Neoplasia syndrome type 2 (MEN 2)
- Have had pancreatitis (talk to your doctor—it may still be possible)
- Have severe stomach or intestinal problems
- Have type 1 diabetes (these are not insulin replacements)
Important Considerations
Long-Term Commitment Required
These medications work while you’re taking them. Most people regain two-thirds of lost weight within a year of stopping. Think of it like blood pressure medication—it manages a chronic condition but doesn’t cure it.
Cost and Access
These medications can be costly without insurance. Most plans cover diabetes use; weight management coverage varies widely. Check insurance coverage and ask about manufacturer savings programs before starting.
Lifestyle Still Matters
Maximum benefit requires healthy eating, regular exercise (especially for preserving muscle), adequate protein intake, and good sleep. These medications enhance—not replace—healthy habits.
Emerging Research
Research is exploring potential benefits beyond diabetes and weight loss, including fatty liver disease, sleep apnea, Alzheimer’s disease, addiction, and kidney disease. While promising, these uses are still investigational.
The Bottom Line
GLP-1 medications represent a genuine breakthrough in treating type 2 diabetes and obesity, with weight loss approaching surgical results and proven heart benefits. However, they require long-term commitment, can have significant side effects, and are expensive. They work best combined with healthy eating, regular activity, and lifestyle changes.
If you’re struggling with type 2 diabetes or weight that hasn’t responded to lifestyle changes, discuss these medications with your healthcare provider. Come prepared with questions, be honest about your concerns, and understand both the benefits and realities of long-term use.
Important Note: This guide is for educational purposes only and should not replace professional medical advice. Always consult with your healthcare provider before starting or stopping any medication. Individual results vary, and what works for one person may not work for another.

